Are MCAS & Long-Covid the Same Thing?
Do you, or someone you know, struggle with post viral syndrome after having COVID, otherwise known as long-haulers syndrome? We’ve recently passed the 3 year anniversary of the WHO declaring COVID-19 a global pandemic, and while the emergency state has ended, and there seems to be a downward trend in hospitalizations and deaths week over week, we’re only beginning to realize the unfortunate long term implications of surviving the virus.
Some individuals who contract COVID-19 are experiencing symptoms like extreme fatigue, brain fog, chest pain and palpitations, shortness of breath, headaches, sleep disruptions, GI issues, and even rashes that continue on for weeks after the initial COVID-19 infection has cleared up - and in many cases these are even lasting for months, or years. These symptoms tend to also worsen after any sort of physical or mental exertion. The medical community has termed this “Long-COVID” or “COVID Long-Hauler Syndrome.” In fact, a surprising rate of about 30% of COVID-19 patients experiences these long-term symptoms after the initial COVID infection. It also resembles the symptom list of those living with Mast Cell Activation Syndrome (MCAS).
Studies are now suggesting that there is a connection between long haulers and MCAS, finding that the symptoms of long haulers occur because the COVID-19 virus actually triggers mast cells to activate (MCAS) and the subsequent cytokine storms. “Long COVID’ describes post-COVID-19 syndrome when symptoms persist for more than 12 weeks after initial infection with no alternative diagnosis. Both mast cell activation syndrome and long COVID cause multiple symptoms. It is theorized that COVID-19 infection could lead to exaggeration of existing undiagnosed mast cell activation syndrome, or could activate normal mast cells owing to the persistence of viral particles.”
The reason why this is so important is because with conditions like MCAS, it is rarely just one underlying root cause that leads you there. Mast cells play an important role in your immune system and nervous system, and they become hyperactive when there is too much going on in your body at once, like excessive pathogens, toxicity, stress, trauma, radiation, or allergens. When it comes to complex conditions like MCAS and long-haulers, healing gets easier when you focus beyond whatever tipped your health over the edge. If you are wondering why you’re all of a sudden dealing with a host of symptoms that come and go since you’ve had COVID-19, this post may give you insight.
What Are Mast Cells? What Do Mast Cells Do For The Body?
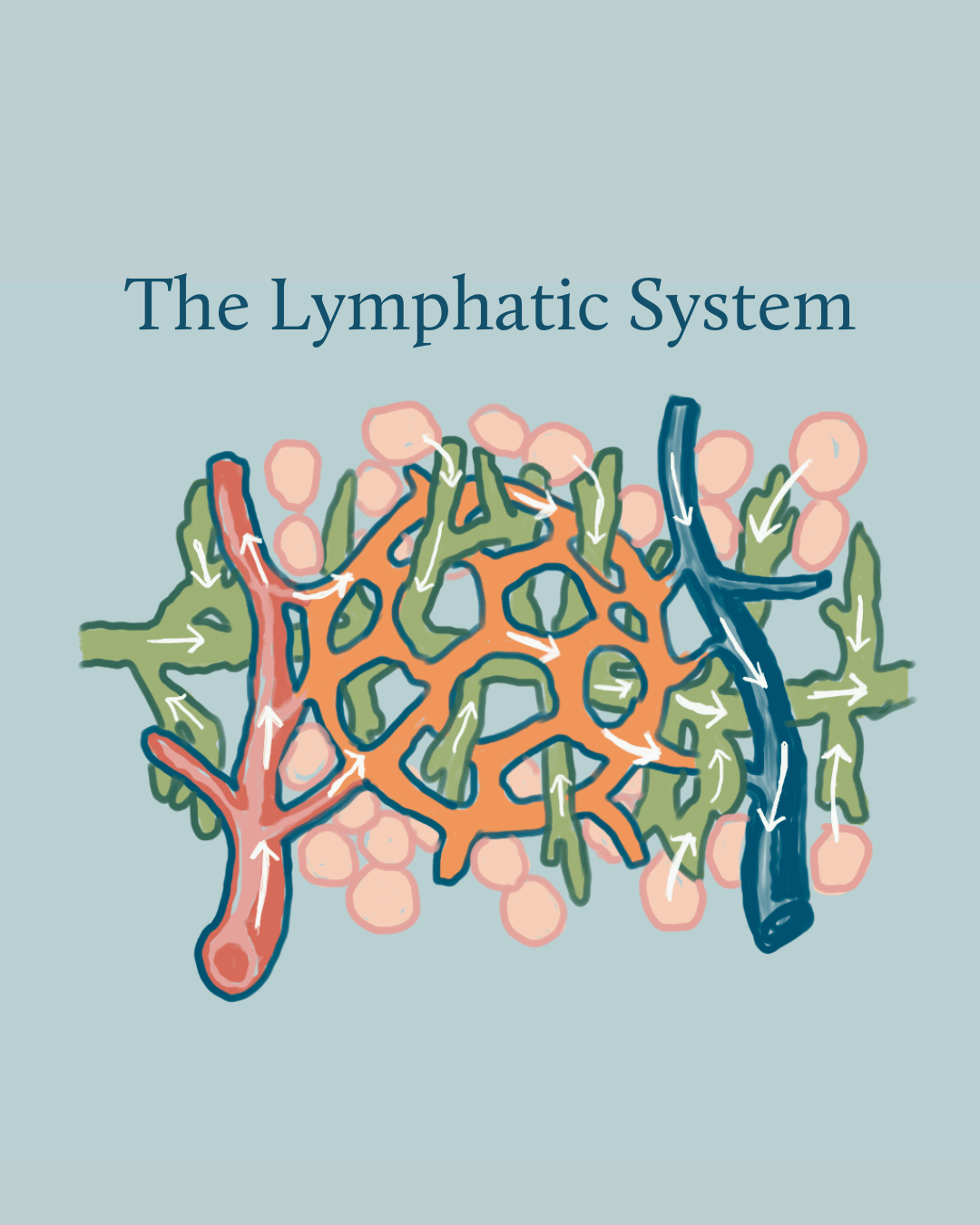
To better understand how MCAS and Long COVID may be related, it’s first important to know what mast cells are, and their important functions within our body (check out our Free Guide on MCAS). Mast cells are part of the immune system, and are found in connective tissues that most commonly interact with our external environment, so think respiratory and digestive tracts, but they can also be found in our nervous and circulatory systems.
Mast cells play an important part in our line of defense against pathogens. They are the alarm bells that alert your immune system to dangers and threats, causing a protective inflammatory cascade to contain the threatening substance or pathogen within your body so it cannot harm you further. This is what happens when you get bit by a bug and it swells, or have seasonal or food allergies. They also help fight off viruses, bacteria, fungus, and parasites.
Mast cells want to protect you, but sometimes they can become hyperactive and overly sensitive. When this happens, they will react to non-pathogenic or non-threatening stimuli but mounting the same level of response as it would give to a pathogen or a true threat where they release elevated amounts of histamine, proinflammatory cytokines, and hundreds of other chemicals and mediators that cause confusing and debilitating symptoms. This is known as Mast Cell Activation Syndrome.
MCAS Cases Are Rising, But Why Now?
Decades ago, Mast Cell Activation Syndrome wasn’t considered a health condition. In fact, MCAS diagnostic criteria was only first proposed in 2010 and then further refined in 2019, meaning most physicians have never been taught about it. It is still often difficult for doctors to diagnose given the number of symptoms and the erratic way they present. If you are lucky enough to find a physician who has heard of MCAS, most of the time they do not know how to treat it. Or they spend years trying to confirm you are positive with unreliable testing methods known to produce false negatives, despite you clinically having so many signs and symptoms.
Prior to the pandemic, there was an estimate that as many as 1 in 5 people has some degree of mast cell activation. MCAS cases are on the rise due to the enormous amount of toxins and stressors in our current environment, filled with the everyday use of plastics, pesticides, chemicals, toxic ingredients, fragrances, and preservatives. On top of this, we’re exposed to high amounts of emotional and psychological stress daily. Many of us have stealth pathogens we co-exist with, like parasites or tickborne infections. All of these things change the way our DNA functions and expresses, and makes us more susceptible to illnesses.
Our mast cells are overstimulated from the abundance of “foreign invaders.” This causes the mast cells themselves to become dysfunctional and wreak havoc in the body at an increasingly high rate among individuals.
While accumulation of toxicities can cause MCAS, countless other factors can trigger MCAS flare-ups:
Parasites
Stress
Lack of sleep
Chemicals (Ingredients in personal care products, cleaners)
Certain Foods
Antibiotics or medications
and Viruses
Cases Of Long-COVID Are Rising
By now, most people have come into contact with the COVID-19 virus. Some people show no signs of infection, while others have unfortunately lost their lives from it. As mentioned earlier, we’re seeing nearly 30% of COVID-19 patients experiencing long term, long-hauler symptoms.
While most Americans believe the worst is over, we haven’t yet experienced the brunt of the rising cases of Long-COVID and the health challenges that come with it. The current healthcare system is not set up to help the influx of people seeking answers and treatment for their many different symptoms. Healing these types of disorders is complicated, especially if you are not trained in MCAS and its associated root causes and triggers.
There has been a skyrocket of cases of long haulers brought on after COVID-19. Another way to view long haulers is that your body is in a prolonged healing crisis, where it cannot complete the healing phases of the acute illness and instead stays in a prolonged state, producing endless cytokine storms. This can happen because of your underlying toxicity, trauma, previous infections, and genetic predisposition.
MCAS Symptoms & Long-COVID Symptoms Are Identical
New research is now suggesting that these Long-COVID symptoms may not actually be a direct result of the SARS-CoV-2 virus itself, but they may be caused by hyper-inflammation caused by mast cell activation (MCAS).
One study showed how mast cell activation symptoms were increased in Long-COVID patients and mimicked the symptoms and severity reported by patients who have MCAS.
Is COVID-19 Triggering Your MCAS?
Given the trend of increasing cases for both MCAS and Long COVID, and the overlap in symptoms, Long-COVID could actually be the result of the COVID-19 virus triggering your MCAS.
It is not uncommon for mast cells to dysfunction following a period of physical or psychological stress, such as fighting off COVID-19. Mast cells then begin to overreact to things that aren’t actually a threat to the body, and didn’t cause issues for prior to a COVID infection. These non-threatening stimuli may include fragrances, foods, personal care products, sounds, physical activity, etc. Because of this over reactivity, mast cells now treat these stimuli like a pathogenic threat and overproduce pro-inflammatory molecules, contributing to symptoms like fatigue, brain fog, headaches, and joint/muscle pain, etc.
What to do if you have Long-COVID Symptoms?
1. Try Supplementing an Antihistamine
If you think you are struggling with Long-COVID, natural antihistamines like Quercetin, Stinging Nettle, Chinese Skullcap, Reishi, Butterbur, and Triphala could help with pain relief for the time being. In one study, 51 of 53 patients were considered a clinical cure using antihistamines, getting them back to a pre-infection health baseline within 2 weeks.
While over-the-counter mast cell stabilizing medications could help in the short term, getting to the root cause of what’s causing your mast cells to be hyperactive and cause all of that histamine is key to helping your body to heal.
2. Address Toxicities and Detox Your Body
Detox has become quite the buzz word lately, but there are right and wrong ways to approach this. When we’re talking about detoxification, this means supporting your to eliminate any harmful toxins safely from your body, like mold mycotoxins, and addressing Lyme disease, cleansing parasites, and living a non-toxic lifestyle.
This can be a complicated and emotional process, and should be done carefully and with a professional in order to minimize detoxification side effects. Make sure you always support your drainage pathways for at least 60 days before you start any detox or cleansing protocols. By alleviating the toxic burden on the body, you are supporting your body in a way that allows it to get out of the healing crisis and return to homeostasis so that it is no longer overreacting to non-pathogenic stimuli.
3. Heal Your Gut
70-80% of your immune system resides in your gut. If you are experiencing MCAS flare-ups, there are most likely underlying gut issues that need to be corrected. These gut issues could stem from leaky gut & food sensitivities, candida overgrowth, dysbiosis, chronic stress, or infections from other bacteria or viruses. Healing these will also help to calm your mast cell activity. We can help you to determine where to focus your effort and give you options for testing in order to provide a personalized protocol, so you’re not trying to recover from an issue that isn’t even causing an imbalance in your body.
4. Work with a Mast Cell Expert
Most conventional doctors don’t know how to deal with MCAS properly because they’ve never been trained to. You need to work with an MCAS expert that not only knows the ins and outs of addressing MCAS and other chronic illnesses, but one that has also been through it personally.
Living with MCAS can be physically, emotionally, and mentally draining. I know because I’ve been there, but remission and having more good days than bad ones is possible. I learned how to overcome MCAS by getting to the root causes. Getting functional medicine lab testing done is a good starting point. We investigate your genes, toxic burden, nutrient status, and pathogens.
If you believe you have MCAS, please read our article, ‘7 Tips for Living with Mast Cell Activation Syndrome (MCAS) That Will Give You Hope.’
Overcome Your Chronic Symptoms & Heal Holistically
Are you looking to get to the root cause of your symptoms? We can help you.
We use holistic approaches and functional medicine lab testing to investigate what is triggering your chronic symptoms so you can address them at their source and start to feel better faster. Our health coaches are masters at guiding the healing of multiple root causes in a personalized order that gets you wellness results that last. We also help you maintain good health and minimize your disease risks.
by sarah southerton
Certified Integrative Health Practitioner (IHP2) & Functional Medicine Health Coach
I specialize in helping people heal chronic illnesses and achieve optimal health. After my own battle with Ehlers Danlos Syndrome (EDS), Lyme disease, Mast Cell Activation Syndrome (MCAS) and Post Orthostatic Tachycardia Syndrome (POTS), I was thrust into the world of alternative medicine, herbal healing, and low-tox/low-stress living. I have since restored my health and no longer suffer with debilitating symptoms and I’m passionate about help other people who are suffering, so they can feel better a lot faster than I did.
Disclaimer: The information on this website is for general information purposes only. Nothing on this site should be taken as healthcare advice for any individual case or situation. This information is not intended to create, and receipt or viewing does not constitute, an healthcare professional-patient relationship. We do our best to keep information accurate and up to date, however mistakes do happen, and we cannot make guarantees regarding the accuracy of our information. We are not liable for any information on this website or your reliance upon it.